As a child I was athletic, adventurous and full of energy. As a high school teenager, I discovered the thrill of learning in the highly competitive academic climate of Princeton, NJ. I had high hopes for college, with dreams of going to the top of whatever field I would grow to love. This was before I came down with ME/CFS (Myalgic encephalomyelitis/Chronic Fatigue Syndrome).
Brain Fog & Visual Disturbances
In 1987, I attended a small liberal arts college in the Chicago suburb of Wheaton, Illinois. Not long after my arrival to the campus I began to experience a constant malaise feeling, with a sore throat, swollen glands and some tiredness. That waxed and waned for a while, but then my serious downfall came during my junior year, 18 months later. My two most debilitating symptoms were, what we in our ME/CFS culture refer to as the “brain fog”; and I also had painful visual disturbances that made it almost impossible to read. When I talk about brain fog I mean that I would have a difficulty understanding language and speaking. I struggled to read others emotions and to feel my own. It felt as if a tight ace bandage was wrapped around my brain and the pressure was a strange type of painful. I felt trapped inside my head unable to connect with the outside world. At one point, I was working in a bookstore and a customer was speaking to me in English but I couldn’t understand her – it was as if she was speaking a language completely foreign to me! At that point, I feared a brain tumor. A subsequent MRI showed no abnormalities. This would come and go throughout my life unexpectedly at what seemed like the most random times.
My optometrist saw that my eyes were spasming and turning inward after a small amount of near focusing. She was the one who ordered the MRI – believing my ocular symptoms to be a possible sign of the beginning stages of MS. Once that was ruled out, she gave me prism glasses in an attempt to relieve some of the stress of reading, but my prescription changed so often and was so baffling that there wasn’t anything she could prescribe that helped. I had to find ways to manage my schooling without a cure.
I would start out each semester with “A’s” and a full load and as I hit each mid-semester my eyes and brain would fail me and my missing assignments would cause my grades to tank. By my senior year, I was just dragging through, having dropped any unnecessary classes and minors in order to just graduate with a bachelors degree and one graduate class. I had hoped that after I graduated and I was able to rest my eyes, I would be able to lead a normal life. Maybe I would even be able to finish that graduate degree that I had managed to start.
Severe Disability of ME/CFS
But the following winter I got worse. I had dizzy spells and often needed help walking from my bed to the bathroom. Most days I would have just enough energy to brush my teeth, shower and dress. Then I would have to go back to bed. My brain fog continued. I looked completely fine on the outside and on a rare occasion I would feel well enough to venture out and be with friends. But it always came back to the same situation – me in bed waiting for the illness to lift. Eventually, I could no longer stay in my apartment with my friends. My health insurance was cancelled. I had to save up to pay for doctor visits which invariably ended with them telling me that it was psychosomatic. I saved up enough to see a psychologist who said that it wasn’t psychological at all – that it was an undiagnosed illness… So hundreds of dollars for contradicting information.
How Doctors Should Treat Patients with ME/CFS
As an aside, I would like to say that these experiences would have been much more tolerable if the doctors I saw had simply admitted that they didn’t know what was wrong with me. Doctors are in a powerful position and should offer respect in a way that dignifies those who are suffering and pay so much to see them, even if their symptoms are confusing and difficult to diagnose. There have been many doctors who have contributed to my suffering both emotionally and by refusing medical care to me. For the few who were kind, respectful and willing to read the research and try new therapies, I will be writing an acknowledgement page with their names and contact information.
Resting, Waiting & Pacing
Eventually I did find a doctor in the Chicago area who told me I wasn’t crazy and that I might have a condition called CFIDS (Chronic Fatigue and Immune Dysfunction Syndrome). Had I not gotten this information, I might have caused myself more damage that could have been irreversible. I went to back to South Florida to live with my aunt and uncle who offered me a place to rest and recover. Medications that were prescribed to me to support my brain and energy levels were Wellbutrin and Synthroid. I was also given a natural multivitamin supplement to take. (I don’t remember what was in it.) I was told to rest when my body was tired. After about three months of complete rest, I felt well enough to try to work and got a job as a youth and children’s pastor at a church in South Florida. I was able to manage that for about a year and a half, but eventually the pace of full-time work was too much for me. I went to live with my parents and worked part-time again.
I got a teaching certificate in the meantime and when I felt strong enough again, I began teaching middle school at a small private school. Looking back now, I know that teaching could have only sustained me for so long, because having an immune deficiency and working with kids resulted in an inordinate amount of sick days. I had to resign from teaching in the middle of the year breaking my contract without proof of my disability. Later that year I married my husband and started a new life working office temp jobs.
Estrogen & ME/CFS
It’s also worth noting that my body didn’t handle estrogen-based birth control pills well at all. I felt like I was losing my mind with anger and all kinds of mood swings, so I became pregnant not long after we were married. Interestingly, most of my ME/CFS symptoms subsided during pregnancy…
Life with ME/CFS ~ Social Barriers
So my life went along, with me staying at home with our daughters and working part-time off and on and doing various volunteer projects as I felt well enough. We lived on one income, my husband worked hard to support us and I don’t know what we would have done if that hadn’t been enough. (It was only in 2015 that ME/CFS was recognized as a legitimate illness with social security for disability support.) I was able to manage a semi-normal life, but I was never able to work full-time again and have felt a great sense of loss in my lack of connection and achievement in a career. My friendships have suffered when my flare-ups have come. And there’s a psychological barrier for me to commit to people or events on a regular basis because I hate to be unreliable. Anyone who suffers with ME/CFS knows this is one of our worst problems because of the loneliness and misperceptions it causes.
I didn’t tell doctors about my symptoms because I didn’t have an official diagnosis and it put me at risk for them to disbelieve anything else I told them. I tried hard to find a different way to explain what was wrong with me, hoping that one day we’d figure it out. The words “chronic fatigue” didn’t seem to come close to what I was experiencing. It often felt more like chronic dying from the inside of my cells outward… (Some of you know what I’m talking about.) So I saw doctors for basic care such as getting an antibiotic when I had an infection, regular blood work, mammograms and paps, and for anything out of “my ordinary”. I noticed that I was sensitive to alcohol, airborne chemicals and mold, so I learned to avoid these things over the years. But more recently I hit an unexpected downward spiral and my ME/CFS symptoms lasted for months and months without relief. I realized that if I was going to get better, I had to do my own research in those rare moments when I had enough energy to think. I did it from my bed. After all, it was 2016 and I had the full search power of Google and the Internet now.
How I began to find answers about my brain fog…
I started with my worst symptom: the brain fog. As an educator I had studied a bit about special needs and the symptoms people on the autism spectrum experienced. My brain fog felt a lot like bouts of temporary autism. Although my brain fog would come and go, it seemed very similar. So my Google searches brought up a UK doctor who treats autism. At the time, she was talking about the genetic mutation or “snp” MTHFR. The theory goes that people with certain MTHFR snps are slower in processing B12 and folic acid to make an important chemical called L-5-methyltetrahydrofolate or L-5MTHF for short. L-5MTHF is the metabolically active form of folic acid that plays many necessary roles in the body to maintain health. It provides the “methyl” to regulate DNA synthesis and repair, to detox from chemicals (including heavy metals such as mercury, lead, arsenic and tin), to metabolize dopamine, epinephrine, serotonin, estrogen & histamine. Could my neurological symptoms be caused by neurotransmitter imbalances and the inability to metabolize toxins? It was worth a look.
I continued my search for doctors who were knowledgable about the MTHFR snp. Soon one of the leading researchers in nutrigenomics and methylation, Dr. Ben Lynch, popped up on my Google search. He takes relevant research on genetics and biochemistry and helps doctors and patients bring that knowledge into practical protocols that improve patients’ health. I wanted to know if I had any genetic predisposition for a MTHF deficiency so I took the 23andMe genetic test, waited the six weeks to get my data and then plugged it into Dr. Lynch’s Strategene tool to see how my genetics may be affecting my biochemical pathways. [Dr. Lynch and Seeking Health now have their own genetic testing in their new Strategene product that includes many more important snps, including IDO2, which is being researched as ME/CFS inflammatory pathway.] Sure enough, I did have a few snps that can slow the production of MTHF, but I also found out so much more looking at several other snps I hadn’t known about before, such as COMT, NOS, VDR (Vitamin D Receptor ~ I always got sicker in the fall and winters, especially when living up north), FUT2, PEMT, DAO, SOD2 and many more. Dr. Lynch maps genes out on their biochemical pathways to show how compounds are metabolized and feed into each other to create biochemical reactions and functions in our bodies. Some of these pathways need help with environmental adjustments such as the air we breathe, water we drink or the foods we eat. Some have problems related to viral loads or toxin levels. Often you can help a particular pathway to speed up or slow down by adding a particular supplement. But all in all, it was a game-changer for me to see the whole picture laid out visually.
Nutrigenomics ~ the Strategene Report
Below is a sample page of the pathway that shows how certain snps are related to the manufacture and metabolism of neurotransmitters: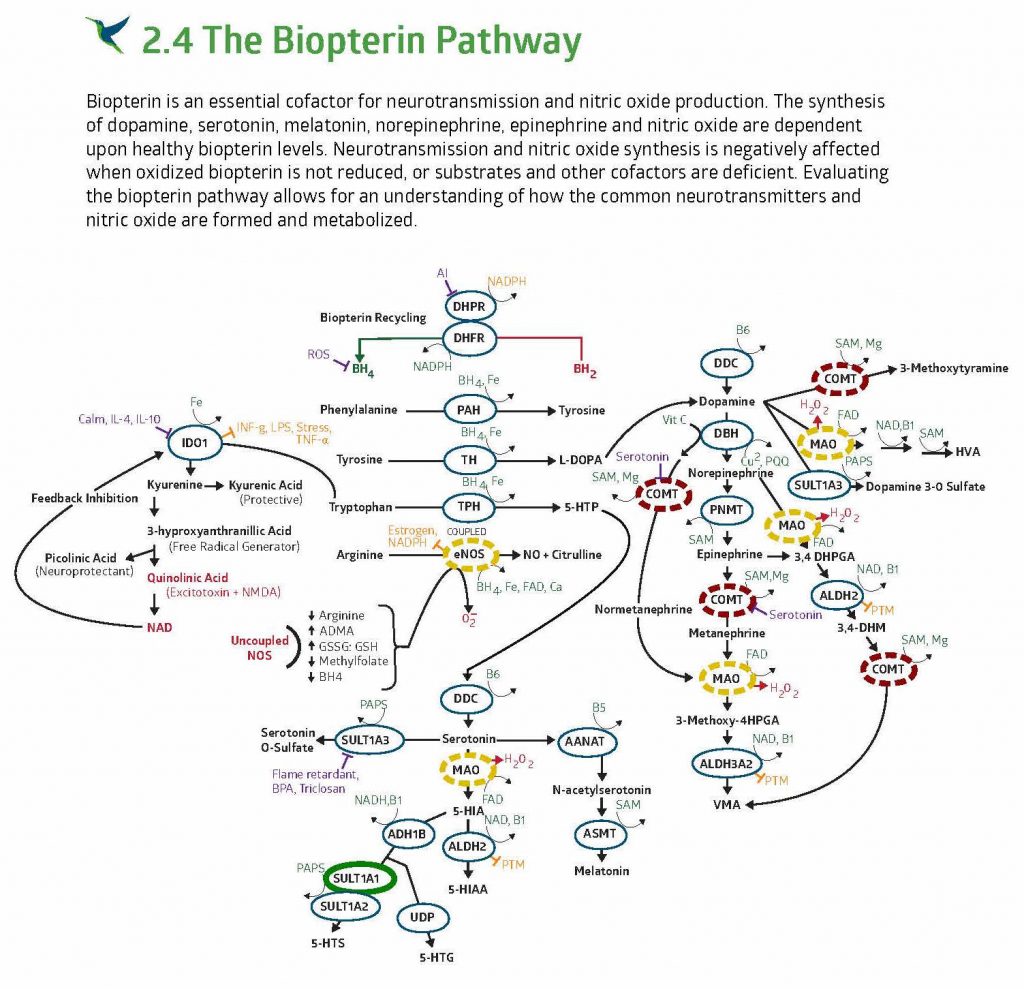
There is much more information in the report and an entire courses that Dr. Lynch has developed to teach us how to use this report, medical history, symptoms and clinical tests to figure out how find individual optimal health. His new book Dirty Genes, takes much of this information and puts it in a way that’s very helpful and easy to understand.
Myalgic Encephalomyelitis Specialist in Florida
While I was busy learning about nutrigenomics and experimenting with various supplements, I was on a two-year wait list to see a doctor at Dr. Nancy Klimas’ clinic at Nova Southeastern University in Davie, Florida. One day I got the call that they had added more clinicians and soon I was on my way to my first visit to see an ME/CFS specialist.
It involved a review of long health history inventory, specialized immunological blood work and a two hour evaluation with the clinician. The first thing I noticed was that they took my illness very seriously and they were experts in this disorder. They are in the middle of a genetic study for ME/CFS and so my clinician was impressed with my Strategene report and recognized Ben Lynch’s name. She ordered tests for active viruses, Lyme disease, and other things and she told me to see a neuro-ophthalmologist to rule out any other underlying ocular disorders. When I showed her the SeekingHealth.com site where I buy most of my supplements, she was thrilled with the liposomal and lozenge options as well as the formulations of her most recommended supplements.
My natural killer cells were deficient and inflammation was high.
After the six-week laboratory process for my immunological blood work, my results came in. They have a test where they take my natural killer cells and put them in a one-to-one fight with viral cells. They figured out the efficacy of my NK cells. My NK cells were only 8% effective in killing a viral cell. So that explains why I’m always getting sick. It explains why I got shingles out of the blue at the age of 47 and I have a chronic active Epstein-Barr virus plaguing me. She called this an acquired immune deficiency. Then there are the autoimmune markers. They look for 18 different inflammatory markers and can tell whether they are coming from mast cell (histamine response), active viral load or the gut. My markers were high for viral load and some for the gut, so their treatment involved probiotics, continuing a bovine colostrum powder (that Dr. Jess Armine had recently prescribed for my daughter) and an antiviral that does well at crossing the blood-brain barrier for EBV and a few others. I talked her into letting me wait on the antiviral because I had a bad reaction to a different one a few years ago and so they are recommending a reishi mushroom extract that is also believed to strengthen NK cell response. If we don’t see results with the reishi, then I will being taking the antiviral.
[Update] After 8 months on LDN and the reishi mushroom extract, my NK cell function was in the normal range and all 18 of my cytokine (inflammatory) markers tested dropped to the normal range!
Low Dose Naltrexone helped my ME/CFS brain fog.
They had given me a prescription for something called low dose naltrexone (LDN) during my first visit. I was afraid to try it because I’m often sensitive to medicines. But my brain fog was still debilitating and I asked her in my second visit if was anything I could take for relief. She said to take the LDN. I convinced her to give me a tiny dose so that I could work up to the recommended dosage. Later that week I started into a bad brain fog and decided to risk it. Within 20 minutes of taking my first dose, I felt my brain fog lift! Nothing had ever taken away that brain inflammation before! I know that this doesn’t work like that for everyone, but it has completely changed my life. In the low doses, it modulates immune response and therefore inflammation and pain.
I still crash. I still have terrible eye pain that keeps me from pursuing a graduate degree or new career or even enjoying a good fiction novel. My health’s not reliable enough to be employed on a regular schedule. But I am much better. I have many good days and I can enjoy my loved ones and pace myself to do some important things in my life. I’m reaching out to those who also suffer and offering what I know, with hope that those researching tirelessly will soon find a cure.